Healthcare cybersecurity services securing patient data & uptime with MDR, identity-first security & ROI tips for USA, UK, Canada, Australia.
Hospitals don’t just deliver care—they safeguard lives, identities, and payments in a nonstop threat environment. Ransomware hits at 2 a.m., legacy devices quietly expose networks, and compliance audits arrive when teams are already short-staffed. Every disruption risks canceled surgeries, diversion to other facilities, and patient harm. The promise of healthcare cybersecurity services is simple: protect patient outcomes and keep revenue flowing with measurable, repeatable controls. Think identity-first access, end-to-end encryption, proactive detection and response, and disaster recovery that works under pressure.
This guide turns best practices into a practical plan for Tier One markets. You’ll see case studies, quick-scan tables you can take to the board, and micro-CTAs to move from “good intentions” to “operationalized outcomes.” Whether you run an NHS trust in Manchester, a regional health system in Texas, a research hospital in Toronto, or a private network in Sydney, you’ll learn how to cut risk, prove compliance, and grow digital services patients trust. The playbook: standardize controls, automate evidence, segment critical systems, and drill your response. Security that’s visible and auditable speeds partnerships, payer contracts, and clinical innovation—without adding overnight heroics.
Creating Cyberthreat Immunity in the Healthcare Industry: Protecting Hospitals and Enterprises in Tier One Markets
“Cyberthreat immunity” isn’t invincibility; it’s resilience by design. A large US multi-hospital network built immunity in three moves: (1) identity-first controls around EHR, imaging, and pharmacy apps; (2) immutable backups and rapid restore tests; (3) 24/7 managed detection and response across endpoints, cloud, and medical networks. When a credential-stuffing wave hit patient portals, step-up MFA and automated lockouts kept clinics open and patient satisfaction steady.
Immunity Building Blocks
| Capability | Why It Matters | Metric to Track |
| IdP + MFA + Conditional Access | Stops account takeovers | Risky sign-ins ↓, MFA fatigue alerts |
| Network Segmentation & ZTNA | Limits lateral movement | Segmented subnets, blocked east-west |
| NGAV/EDR + MDR | Detects & contains fast | MTTD/MTTR, isolation time |
| Immutable Backups (Quarterly Drills) | Survives ransomware | Restore success %, RTO/RPO met |
| Evidence Automation (GRC) | Passes audits faster | Hours saved, audit findings ↓ |
Mini Case – UK Trust: After segmenting imaging (PACS) and enforcing device posture checks, the trust reduced high-risk events by 58% quarter over quarter and cut pen-test remediation cycles in half.
Key Tip: Start where clinical risk meets business risk—EHR access, imaging, and medication management.
Explore more details here → Run a 90-minute tabletop to validate isolation procedures and restore steps.
What You Can Do to Enhance ROI and Secure Patient Data with Healthcare Cybersecurity Services
ROI in healthcare security shows up as uninterrupted care, fewer diversions, and lower insurance scrutiny. A Canadian hospital coalition mapped top 10 controls to financial outcomes—reduced breach likelihood, faster payer audits, and improved service uptime. Result: expansion of telehealth with minimal extra staffing.
Control-to-Outcome Map
| Control | Cost Driver Affected | Tangible ROI |
| SSO + MFA for EHR & portals | Helpdesk resets, fraud | Ticket volume ↓, fraud refunds ↓ |
| Email Threat Protection | BEC & phishing | Fewer incidents, staff time saved |
| Patch Orchestration (Ring-based) | Vulnerability exposure | Mean patch time < 7 days |
| ZTNA for Vendors | Third-party risk | Faster onboarding, fewer exceptions |
| Immutable Backups | Ransomware impact | Reduced downtime penalties |
Mini Case – Australia: A private hospital group moved from VPN to app-level access with device posture checks. Clinical apps loaded faster, contractor access shrank from days to hours, and security questionnaires moved from red to green.
Result: Risk fell, and revenue grew as partnerships accelerated.
Takeaway: Tie every control to uptime, audit hours saved, or avoided write-offs.
Key Cybersecurity Challenges for the Healthcare Industry: Insights for CIOs and Decision-Makers in the USA and UK
Healthcare faces five stubborn headwinds: (1) legacy systems with long device lifecycles; (2) 24/7 availability requirements; (3) complex third-party ecosystems; (4) sensitive ePHI/PII under multiple regulations; (5) talent shortages. A US academic medical center consolidated from seven endpoint agents to two (XDR + DLP), introduced privileged access management for admins and biomedical engineers, and codified cloud guardrails. Mean time to respond dropped by 41% and weekend pages declined by a third.
Challenge Prioritization
| Challenge | Risk | First Move |
| Legacy OS & imaging | Lateral movement | Micro-segmentation, VDI isolation |
| Vendor/IoT sprawl | Unmanaged access | ZTNA + signed connectors |
| Email & portal fraud | Patient trust | DMARC, advanced phishing defense |
| Evidence fatigue | Audit delays | Automated evidence collection |
| Staffing gaps | Alert backlog | MDR with clear runbooks |
Key Tip: Standardize the 80% (identity, email, endpoint, backups, evidence) and specialize the 20% (OT/IoMT, research networks).
Explore more details here → Document “gold controls” per domain with KPIs and owners.
Safeguard the Patient Experience with Enterprise-Grade Cybersecurity Services in Canada and Australia
Patient experience now includes “secure by default.” When portals feel safe and fast, telehealth adoption rises. A Toronto network launched passkey support for patients, reduced password resets by 35%, and saw portal use climb. In Sydney, a system introduced device posture checks for remote clinicians—no compliant device, no access—cutting suspicious sign-ins and smoothing audits under CPS 234 and the Essential Eight.
Experience & Trust Matrix
| Experience Pillar | Security Control | Trust Signal |
| Fast access | SSO/Passkeys | Fewer lockouts |
| Safe messaging | DLP + encryption | No misdirected mail |
| Resilient services | DR drills | Fewer diversions |
| Transparent privacy | Consent mgmt | Fewer complaints |

Secure Patients’ Health Records with End-to-End Encryption for ROI and Compliance
End-to-end encryption (E2EE) closes gaps between clinics, pharmacies, labs, and cloud apps. Combine transit encryption (TLS 1.2+) with field-level encryption for ePHI at rest, keys in HSMs, and strict key rotation. A UK radiology practice encrypted images and reports at the field level, aligning with NHS DSPT and ISO 27001, and cut data-handling exceptions during audits by 70%.
Pros & Cons
| Aspect | Pros | Cons |
| Field-level encryption | Granular protection | App complexity |
| HSM-backed keys | Strong assurance | Cost/skills |
| E2EE messaging | Low leakage risk | Vendor support varies |
Expert Insight: Make key management product-grade—dedicated owners, tested rotations, and break-glass procedures.
Define a Comprehensive Cybersecurity Strategy for Enterprise Healthcare Growth
A strategy is a contract between clinical needs and defensive reality. Use a three-horizon model: Horizon 1 (stabilize), Horizon 2 (optimize), Horizon 3 (innovate). Tie each project to clinical uptime, revenue protection, and audit readiness.
Strategy Map
| Horizon | Focus | Example KPI |
| H1 (0–6 mo) | Identity, email, backups | MFA coverage 100% |
| H2 (6–12 mo) | Segmentation, MDR, DLP | MTTD < 10 min |
| H3 (12–24 mo) | Zero trust, passkeys, CCM | Audit hours ↓ 40% |
Expert Insight: Publish quarterly “risk-to-revenue” updates for execs—simple trends, no jargon.
Secure Medical Devices to Build Patient Trust and Lead Generation Opportunities
IoMT and biomedical devices often run legacy stacks. The fix is segmentation, strong inventory, and compensating controls. A US pediatric hospital created a device called CMDB, grouped devices by risk, enforced ACLs per VLAN, and mirrored traffic to XDR. Result: fewer false positives and safer maintenance windows.
Device Security Snapshot
| Control | Why | Quick Win |
| Asset inventory | Know exposure | Passive discovery |
| Network micro-segmentation | Limit spread | Risk-based VLANs |
| Signed updates | Integrity | Vendor SLAs |
| NAC/Device posture | Gate access | Block unknown MACs |
Expert Insight: Treat high-risk devices like critical patients—observe, isolate, intervene fast.
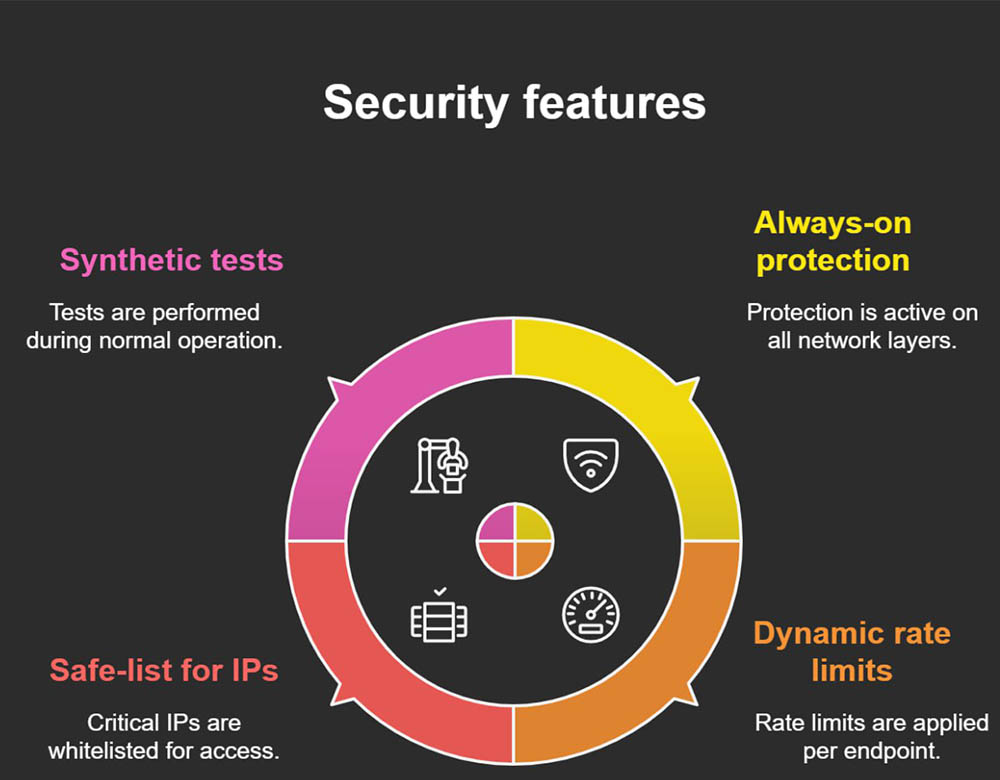
Advanced Web DDoS Protection for Healthcare Enterprises in Tier One Countries
DDoS on a booking portal or telehealth gateway isn’t just IT downtime—it’s missed care. Use layered defenses: CDN-based absorption, behavioral rate-limiting, bot management, and origin shielding. An Australian hospital moved to always-on DDoS protection; during a surge, legitimate traffic kept flowing while attack traffic dropped at the edge.
DDoS Stack
| Layer | Control | Measure |
| Edge | Anycast + WAF | Req/sec handled |
| App | Bot mgmt, CAPTCHA | Challenge pass rate |
| Origin | Auto-scaling, shielding | CPU/utilization stable |
Expert Insight: Practice fail-open for critical patient flows (e.g., emergency contact), fail-closed for admin panels.
How to Prevent Disruption of Critical Patient Services: A Step-by-Step Cybersecurity Guide
- Identify crown jewels: EHR, PACS, eMAR, lab, and scheduling.
- Enforce identity controls: SSO/MFA, conditional access; disable legacy auth.
- Segment networks: Isolate clinical from admin and guest networks.
- Harden email & endpoints: Advanced phishing defense, NGAV/EDR with isolation.
- Backups & DR: Immutable backups, quarterly restores, documented RTO/RPO.
- MDR & SOAR: 24/7 watch + automated playbooks.
- Evidence automation: Map controls to HIPAA, GDPR, PIPEDA, CPS 234, DSPT.
- Drill & improve: Tabletop and live restores; publish results.
Why Protection Against Any DDoS Attack is Essential for Healthcare ROI
DDoS disrupts clinical portals, telehealth, and appointment booking—directly impacting revenue and reputation. Mitigation reduces cancellations, call-center spikes, and downstream rescheduling costs. Pair protection with cache strategies for static content, and prioritize emergency access pathways.
Checklist
- Always-on L3–L7 protection
- Dynamic rate limits per endpoint
- Safe-list for critical IPs (ambulance services, labs)
- Synthetic tests during peacetime
What Strictly Necessary Cookies Mean for Patient Data Privacy in Healthcare Apps
“Strictly necessary” cookies enable core functions—authentication, load balancing, and consent storage. They don’t track marketing. In UK and EU contexts, they’re typically exempt from consent banners, but must be disclosed. Keep them minimal, secured (HttpOnly, Secure, SameSite), and documented.
Quick Guide
- Limit to auth/session, not analytics
- Rotate session IDs, short TTLs
- Document in privacy notice
How to Choose a Region for Secure Healthcare Data Hosting in the USA, UK, Canada, and Australia
Pick regions that satisfy data residency and latency. For NHS trusts, keep patient data in UK regions; for Canadian hospitals, prefer Canada-based data centers (PIPEDA). In Australia, align with CPS 234 guidance and state laws. Consider disaster pairing (e.g., UK South + UK West) and key residency via HSMs.
Selection Matrix
| Country | Residency Priority | Pairing Idea |
| USA | HIPAA BAAs, state laws | East/Central |
| UK | NHS DSPT, UK GDPR | UK South/West |
| Canada | PIPEDA/Provincial | CA Central/Quebec |
| Australia | CPS 234, APPs | East/Southeast |
Adapt to a New Digital Future: Case Study of Healthcare Cybersecurity Services in the UK
A London community health trust moved to SSO/MFA, introduced passkeys for staff kiosks, segmented IoMT, and automated evidence for DSPT. Incidents fell 44%, password reset tickets dropped 30%, and audits shortened by two weeks.
Stats Snapshot
| Area | Before | After |
| High-risk sign-ins | 1,100/mo | 420/mo |
| Password tickets | 800/mo | 560/mo |
| Audit days | 20 | 14 |
Key Tip: Pilot passkeys in low-friction areas first (kiosks, shared workstations).
Talk to Our Cybersecurity Expert: Best Practices for US Healthcare Enterprises
US systems juggle HIPAA, HITECH, and payer audits. Best practices: IdP-first design, disable legacy auth, enforce device posture, ring-based patching, immutable backups, MDR with SOAR, and quarterly restore drills.
Tiny Table
| Practice | KPI |
| MFA coverage | 100% |
| Patch latency | < 7 days |
| Restore success | 100%/quarter |
Free Assessment Tools to Evaluate Cybersecurity ROI in Canadian Hospitals
Use a simple calculator: map controls to avoid incident costs, audit time saved, and reduced insurance premiums. Include downtime costs per clinical app and diversion penalties.
Inputs & Outputs
| Input | Output |
| App uptime, RTO/RPO | $ saved per hour |
| MFA & DLP coverage | Fraud/write-offs avoided |
| Drill frequency | Insurance impact |
Key Tip: Share the ROI sheet with finance to co-own the roadmap.
Let There Be Change: Enterprise Cybersecurity Transformation in Australian Healthcare Systems
An Australian health network adopted ZTNA for contractors, enforced passkeys for admins, and automated Essential Eight evidence. With quarterly ransomware drills, they kept clinics operational during two real-world attempts.
Result: Better insurer terms and faster partner onboarding.
Takeaway: Transformation is process + proof. Show monthly metrics to executives.
Challenge / Solution Report: Healthcare Cybersecurity Services ROI in Tier One Markets
Challenge: Rising ransomware, legacy stacks, and regulatory pressure.
Solution: Identity-first security, segmentation, MDR, immutable backups, and evidence automation.
ROI: Fewer diversions, faster audits, reduced fraud, stronger patient adoption of digital services.
Key Tip: Publish a “clinical uptime & security” dashboard with five KPIs: MFA coverage, MTTD/MTTR, restore success, patch latency, and DDoS availability.
Managed Services vs Professional Services: Expert Insights for Healthcare Enterprises in the USA and UK
Managed Services (MS): 24/7 operations—monitoring, patching, backup tests, and incident response. Predictable OPEX and steady KPIs.
Professional Services (PS): Time-bound projects—strategy, migrations, segmentation, and audits. Ideal for transformation phases.
Best outcomes blend both: PS to design the blueprint, MS to run it daily with MDR on top.
Takeaway: Buy outcomes, not tools. Demand monthly evidence and quarterly drill reports.
FAQs:
What is cybersecurity in healthcare and why is it critical for ROI-driven hospitals?
Healthcare cybersecurity protects clinical systems, patient portals, devices, and data from threats that can halt care. Strong controls—SSO/MFA, segmentation, NGAV/EDR, immutable backups, and MDR—reduce downtime, diversions, and write-offs. They also speed payer and partner reviews, cutting friction in revenue cycles. When portals and telehealth are reliable and safe, adoption rises, improving visit completion and satisfaction. Finally, automated evidence shortens audits, freeing staff to focus on patients. In short, cybersecurity safeguards lives and revenue: it keeps clinics open, protects patient trust, and makes digital care scalable without constant firefighting.
What are the 7 types of cybersecurity services used in healthcare enterprises?
- Identity & Access Management (SSO/MFA/IdP). 2) Endpoint protection (NGAV/EDR). 3) Email and web security (phishing, DMARC, WAF/Bot). 4) Network security (segmentation, ZTNA/SD-WAN). 5) Data protection (encryption, DLP, key management). 6) Backup/Disaster Recovery (immutable storage, drills). 7) Monitoring & Response (SIEM/XDR, MDR/SOC). Supporting layers include GRC/evidence automation and third-party risk management. Together they create a defense-in-depth posture that aligns with HIPAA, GDPR/UK GDPR, PIPEDA, and CPS 234 while preserving clinical uptime and patient experience.
What is NHS cybersecurity and how does it protect patient data in the UK?
NHS cybersecurity combines policy frameworks (e.g., DSPT), technical standards, and operational practices to secure trusts, ICSs, and GP practices. Core elements include identity-first access to clinical systems, secure messaging, network segmentation for imaging and labs, robust email protection, and incident response processes shared across regions. Many trusts adopt encryption at rest and in transit, immutable backups with regular restores, and ongoing staff awareness. The outcome is safer data handling, fewer breaches, and faster audits—improving patient trust and enabling digital front-doors like e-referrals and online triage to run reliably.
What are the 5 C’s of cybersecurity and how do they apply to healthcare organizations?
- Confidentiality: Protect ePHI through encryption, access controls, and DLP.
- Integrity: Ensure records aren’t altered via signed updates, checksums, and RBAC.
- Availability: Keep systems online using DR plans, clustering, and DDoS protection.
- Compliance: Map controls to HIPAA, GDPR/UK GDPR, PIPEDA, CPS 234, DSPT.
- Continuity: Drill incidents and restore scenarios to maintain care during crises.
Applied together, the 5 C’s translate into measurable outcomes: lower breach risk, predictable uptime, faster audits, and higher patient satisfaction with digital services.
Which are the best healthcare cybersecurity services companies in the USA, Canada, and Australia?
“Best” depends on your environment, compliance needs, and integration stack. Prioritize providers that prove outcomes: MFA everywhere, rapid isolation times, immutable backups with successful quarterly restores, and automated evidence exports. Ask for healthcare references in your country, a live demo of incident triage, and a data-residency plan. Shortlist vendors who provide co-managed options, medical device segmentation experience, and clear SLAs tied to MTTD/MTTR, patch latency, and restore success. Choose partners who speak patient safety and revenue, not just tools.
How much does healthcare cybersecurity cost for enterprises and hospitals in 2025?
Budgets vary by bed count and digital scope, but think in layers. Baseline (IdP/MFA, email, EDR, backup) often runs as a per-user/device subscription. Add SIEM/XDR, MDR, and DDoS/WAF for 24/7 coverage. Project-based spend covers segmentation, cloud guardrails, and GRC automation. The most effective programs link spend to outcomes—reduced downtime and audit hours saved—so CFOs can see payback. Right-size by standardizing the 80%, then add specialized services for IoMT/OT and research networks.
What are the top healthcare cybersecurity services jobs and career paths in Tier One markets?
High-demand roles: IAM engineer (IdP, passkeys, PAM), detection engineer (XDR rules, UEBA), MDR analyst, cloud security engineer (policy-as-code), biomedical/IoMT security specialist, DFIR responder, and GRC automation lead. Paths often start in SOC or IT security and branch into identity, cloud, or medical device security. Employers value scripting (Python), IaC, detection logic, and evidence automation. Certifications like CISSP, CCSP, GIAC blue-team tracks, and healthcare privacy credentials help—paired with the ability to translate security actions into patient safety and operational KPIs.
What is Sensato cybersecurity and why is it trusted in the healthcare sector?
Sensato is known in healthcare for security services that focus on clinical realities—medical device risk, continuous monitoring, and incident response aligned to hospital workflows. Its emphasis on practical runbooks, biomedical collaboration, and rapid detection/containment helps hospitals maintain clinical uptime. Organizations trust providers like Sensato when they demonstrate deep sector knowledge, clear SLAs, and real-world references—especially around IoMT segmentation, ransomware readiness, and hands-on drills that prove systems can be restored without delaying care.
How do CloudWave solutions help enterprises streamline healthcare cybersecurity?
CloudWave (often associated with healthcare cloud and security services) helps standardize hosting, resilience, and monitoring around clinical apps. Value comes from aligned runbooks, data residency options, backup/DR orchestration, and security operations tuned to EHRs and imaging. For many hospitals, the benefit is fewer vendors, clearer SLAs, and audit-ready evidence that reduces project and compliance friction. When evaluating any partner, request a live demo of restore drills, identity integration, and incident workflows across your most critical clinical applications.
What is the best healthcare cybersecurity services checklist for compliance and ROI?
- IdP/SSO/MFA coverage = 100% (no legacy auth).
- NGAV/EDR with isolation + MDR 24/7.
- Email security (DMARC, advanced phishing defense).
- Segmentation for EHR, PACS, lab, and admin networks.
- Immutable backups with quarterly, witnessed restores.
- DLP + field-level encryption; keys in HSMs.
- Evidence automation mapped to HIPAA, GDPR/UK GDPR, PIPEDA, CPS 234, DSPT.
- Quarterly tabletop and DDoS war-games.
Track MTTD/MTTR, restore success, patch latency, and portal uptime to show payback.
Healthcare cybersecurity services vs traditional IT security: What delivers higher ROI?
Healthcare-focused services deliver higher ROI because they’re built around clinical uptime, IoMT, and regulatory evidence. Traditional IT security can miss workflow realities—shared workstations, device lifecycles, and vendor access. Sector-specific programs prioritize segmentation of imaging/lab systems, strong identity for clinicians, immutable backups, and drills that keep clinics open. They also automate evidence for audits, saving weeks of staff time. ROI shows up as fewer diversions, stable portals, faster payer reviews, and better insurance terms.
Which cybersecurity services are most effective for protecting patient records in the USA and UK?
Start with IdP/SSO/MFA to secure all clinical and patient-facing apps. Add NGAV/EDR with rapid isolation, email security with DMARC and impersonation detection, and field-level encryption for ePHI. Enforce segmentation for EHR, imaging, and labs to limit blast radius. Back everything with immutable backups and quarterly restores. In the UK, align controls with UK GDPR and DSPT; in the USA, ensure HIPAA-aligned policies and BAAs. Measure success through reduced high-risk sign-ins, lower phishing incidents, and flawless restore tests.
